Fast App: Precision is Everything
Yes, it is brain surgery ... so FHC switches to EOS' plastics laser-sintering system to manufacture the patient-specific STarFix platform.
Latest News
March 13, 2013
By Lynn Manning
The patient lies wide awake in the operating room (OR), the top of his draped head bared to the neurosurgeon. A second doctor stands at the patient’s side, lifts the man’s arm, and flexes it gently. The hand and wrist are stiff, with a visible tremor. The surgeon makes a slight adjustment to brain-penetrating electrodes mounted through a starburst-shaped plastic fixture fastened to the man’s skull.“How about now?” the surgeon asks.
The arm is moved again “this time naturally, smoothly, without shaking.
“That’s it,” says the patient, nodding his head with relief.
The procedure is called deep brain stimulation (DBS), and it is has become a lifestyle-saver for people suffering from Parkinson’s disease, essential tremor, dystonia and other neurological afflictions that don’t respond sufficiently to medication alone. Recent studies even point to DBS’ potential in treating dementia, epilepsy and depression.
What makes the story above such a standout is not so much the symptom-relieving surgery “but that the patient was able to move his head during it.
 DBS case led by Dr. Carlos Jaime Yepes at Clínica Las Américas in Medellín, Colombia. Yepes is Latin America’s first neurosurgeon to use the microTargeting Platform. |
That simple movement is the result of some truly “outside-the-frame” thinking in the concept of brain surgery. DBS, while performed effectively approximately 9,000 times a year worldwide, has traditionally involved many grueling hours of awake imaging, target identification and electrode implantation “all with the patient’s head completely immobilized. Securing the head to the operating table via a large, heavy stereotactic frame was felt to be the best way to pinpoint critical brain tissue locations measured in millimeters. Accuracy had to take precedence over patient comfort. Routinely employed since the 1960s, the frames have nevertheless been cited by patients as the most unpleasant part of the entire surgery.
Let’s Lose the Frame
But now a breakthrough invention, the frameless stereotactic platform, is being used in a growing number of DBS procedures around the globe. Anchored to the skull rather than the table, each patient-specific fixture provides dramatic improvement in comfort “while at the same time giving surgeons greater precision for targeting the tools they need to reach trouble spots. Because much of the preparation and planning is done in advance, time in the OR can be reduced as much as two hours, with correspondingly less strain on the patient and lower hospital costs. During a DBS procedure, the frameless system allows patients to move their heads, sit up, write and even walk “all of which helps doctors identify where in the brain is the ideal spot to implant the symptom-relieving electrodes without impairing normal function.
 |  |
| Figs. 1a and 1b. DBS, left, and close-up of STarFix microTargeting Platform mounted on the skull during surgery for a bilateral procedure, right. | |
The genesis of this head-freeing technology came from neurosurgeon Dr. Joel Franck, who was practicing at St. Mary’s Hospital in Lewiston, ME, in the late 1990s. As he worked with traditional stereotactic frames, he recalled his undergraduate studies with cranial-mounted technology on animals and wondered whether the same technology could benefit people as well.
“I was looking for a partner to bring my ideas to fruition,” Franck says. “The development of a new medical procedure is a very time-consuming, iterative process.”
He was pleased to find medical design and manufacturing experts at FHC Inc., just 20 miles away in Bowdoin, ME: “FHC’s experience in both research and clinical realms was very helpful.”
| How DBS WorksAs scientists deepen their knowledge of the biochemistry of the brain, many patients have benefitted from drugs that relieve, or at least reduce symptoms of a number of serious brain disorders. But in some people, the drugs don’t work well enough for them to lead normal lives, or cause side effects that become intolerable. These folks are candidates for DBS, which was FDA-approved for patients with Parkinson’s disease and essential tremor in 1998 and has since gained widespread acceptance from neurologists. DBS involves implanting one or more electrodes in the specific area(s) of the brain that give rise to abnormal symptoms. Continuous electrical current delivered through the electrode often dramatically reduces problems. A battery pack that powers the electrode is implanted in the patient’s chest, much like a heart pacemaker, and the amount of current can be adjusted over time for optimum results. A short video from Norton Health, found online at Vimeo.com/26557359, shows a Parkinson’s patient, initially unable to hold a piece of paper still, completely tremor-free after undergoing DBS. Some Parkinson’s patients may need to continue to take medication after DBS, but at greatly reduced doses. In the case of essential tremor, a reported 80% of patients who undergo DBS have complete relief of symptoms without post-operative medication. The challenge with DBS is identifying where exactly the electrode must be sited to achieve optimum results. While general knowledge about what parts of the brain control what behaviors and functions is now reasonably well known, each person’s physiology is unique and not every internal brain “structure” is clearly visible to the eye—or even CT or MRI scans. What’s more, the brain can actually shift slightly in relation to the skull during normal movement, such as going from standing to lying down. So even the most precise targeting set-up methodology is still an approximation within about an eighth of an inch—which in brain mapping can make a huge difference. A common DBS target, the subthalamic nucleus (STN), for example, is only a little bigger than a green pea, but that is where the electrode must be centered for effective stimulation. Move away from this by just a few millimeters, and the treatment may be less effective. The accuracy issue underscores the importance of “awake” surgery, where the patient can talk—and move, if fitted with a frameless platform—as microdrives carefully nudge test electrodes through clusters of neurons at different depths in the brain. The brain contributes to the conversation as well: Electrophysiological monitoring records the signals from the neurons in each area as the microelectrodes move deeper. Each critical region has its own signature pattern, clearly identifiable with monitoring equipment.
In Fig. 6, each of the four lines of data shows the electrical output from a different functional part of the brain. The target is the STN, where stimulation will relieve the symptoms of Parkinson’s disease. As a test electrode moves down through the top two brain regions (thalamus/reticular nucleus of the thalamus and the zona incerta), the neurologist can see and hear the distinct firing patterns of nerve cells in each. If the electrode goes too deep, beyond the STN target (into the substantia nigra), the pattern changes noticeably—and the surgeon knows to withdraw the electrode slightly back up into the STN. Once the target site is positively identified, the test electrode is withdrawn and replaced with a larger, battery-powered stimulating electrode that will remain in the brain after surgery. No single mechanism has been found to explain exactly why long-term DBS works. It may affect the flow of ions between neurons; some studies also show increased blood flow where electrical current is applied. But thousands of patients around the globe will testify to how DBS has made all the difference in their lives. —L. Manning |
Innovation through Collaboration
“Surgeons can come to us with their ideas, and we will work very closely with them to come up with a practical solution,” says FHC CTO Ron Franklin. “This is exactly how we like to implement our company’s philosophy of ‘innovation through collaboration.’”
Franck and the FHC team initially developed several ideas that relied on mounting, registering and adjusting an existing mechanical holding device.
 Fig. 2. FHC’s WayPoint Navigator Planning Station allows the surgeon to use the patient’s CT and MRI data, in combination with anchor locations on the skull, to confirm target and entry points and create the design for the Platform (in green). |
A breakthrough occurred when the group realized that all they were trying to do was fix an instrument in a known location relative to a target: If you set up three or four anchor attachment points on a person’s skull, you could factor in the person’s CT and/or MRI data to create a custom-formed stereotactic platform that would attach to the anchors and align a microdrive to guide and implant electrodes to the deep brain sites you were targeting. Each unique platform would fuse the patient’s anatomical information with the surgeon’s trajectory plan, so the required approach was built right in. What’s more, if you used materials that could be used inside MR and CT scanners, most of the setup could be done ahead of time “reducing both patient and surgeon time in the OR. The final bonus: Accuracy would be maintained if the patient moved during surgery because the platform would move with him.
How to manufacture such a patient- and procedure-specific product? The emerging technology of additive manufacturing (AM) offered just this kind of “growing to a desired shape” customization that the group desired.
“Development of this unique device technology was greatly enabled by advances in AM that FHC was just starting to take advantage of,” Franck recalls. A boat-modeling process developed by a local marine software design company was adapted into a library of standard, “intelligent” 3D digital models of surgical fixtures that could be easily modified to fit individual patient anatomy data and surgery planning requirements, and then built inside an AM machine.
The resulting customizable interface technology reflects the growing trend toward patient-specific medical devices, and can potentially be used for any type of orthopedic surgery (spinal, long bone, etc., as well as cranial). Dubbed STarFix (Surgical Targeting Fixtures), it was patented within a separate company in 2001 and received approval from the U.S. Food & Drug Administration. FHC, as a licensee of STarFix, employed the technology to develop its microTargeting Platform for cranial neurosurgery, along with its own associated WayPoint Planner software algorithms.
Franck performed the world’s first DBS procedure with the Platform late that same year, and it has since been used in almost 3,000 cranial neurosurgeries worldwide. The STarFix microTargeting Platform received a Gold Medal Design Excellence Award in 2004.
Hospitals and Surgeons Get on Board
The Platform caught the eye of neurosurgeons at Nashville’s Vanderbilt University Medical Center, one of the country’s leading DBS practitioners. Their own work with bone markers and image co-registration helped them intuitively recognize the value of FHC’s technological leap.
“I was delighted with the convenience the Platform afforded me in surgical target planning, ease of use and stability of the frame during the surgery and, most importantly, patient comfort,” reports Dr. Peter Konrad, Ph.D. M.D., director of functional neurosurgery, Vanderbilt University.
In late 2002, Vanderbilt switched most of its DBS surgeries to the Platform, and at press time has performed nearly 600 procedures since. “The Platform’s accuracy is unparalleled by any other frame or frameless system, as reported in peer-reviewed literature,” says Konrad. “Patients who have experienced DBS surgery with both traditional frames and these customized ones have all commented how much more comfortable and tolerable the surgical process is with the latter.”
As word of the Platform spread, FHC switched from an earlier-generation AM machine to laser sintering. “Our first laser-sintering machine served us well for several years, during which we developed widespread medical acceptance for our custom fixtures,” Franklin says. “Published accuracy studies by independent researchers confirmed that we were already in the sub-millimetric range with that machine.”
 Fig. 3. Underlying computer model of bilateral Platform (electrodes will be mounted through top two openings), with two additional ports for side X-ray target confirmation. This 3D data is used to drive the laser-sintering manufacturing process. |
Precision is the holy grail at FHC, which has supported the neuroscience community for more than 40 years through the design and manufacture of specialized microelectrodes, and a broad range of research and clinical instrumentation.
“With brain surgery, the more precise the instrument, the better,” says Franklin. “A prospective study of all patients undergoing DBS with the Platform indicates that this particular device, because of the way it’s made, is about twice as accurate as a standard stereotactic frame.”
Increasing Precision, Demand
But achieving accuracy with the first laser-sintering machine was taking its toll in time and cost. “We were using a lot of expensive virgin powder in our old system, and we needed to increase our throughput as orders for the Platform ramped up,” says Franklin. “Sometimes we had to do rebuilds to achieve the precision we wanted.”
 Fig. 4. The Formiga P 100 laser-sintering system from EOS. FHC switched its primary manufacturing of its polyamide microTargeting Platform to this system in 2011. Fig. 4. The Formiga P 100 laser-sintering system from EOS. FHC switched its primary manufacturing of its polyamide microTargeting Platform to this system in 2011. |
In 2011, FHC decided to purchase a Formiga P 100 plastics laser-sintering system from EOS as its primary manufacturing unit. “The Formiga is smaller, lighter, has a lower cost of use and provides better dimensional accuracy than our previous machine,” says Franklin.
FHC laser-sinters its Platforms from EOS’ PA 2201 FDA-compliant, biocompatible polyamide powder, known for strength and stiffness, good chemical resistance, excellent behavior over time, selectivity and detail resolution. “It’s definitely more economical for us to use EOS’ high-quality polyamide material,” says Franklin. “There’s no overflow of powder during the build process, and the size of the machine’s build chamber is more appropriate for what we manufacture.”
Because consistency and dimensional tolerance are greater with the EOS system, the entire build process and breakout procedures are more refined than before, he adds. “We are able to post-process the holes and mounting features in the fixtures more easily, and do not rely as much on sizing tools as before. Our quality assurance process now takes less time because the Formiga-manufactured devices are closer to the model geometry. We have not had as many rebuilds with the EOS machine as we had previously.”
With orders coming in from all over the world (currently about 500 units per year), FHC has discovered another plus with the Formiga P 100: It can add incoming orders to a build already in process. “We can start one build and then add in a late second-build plate, which is a major benefit,” says Franklin. Still, he notes, accuracy is key: “We have to get an accurate surgical fixture to our users on time and with no errors. Response time to the needs of the doctor is critical.”
FHC typically receives a patient file during the working day, consults with the physician as needed to confirm the design, starts manufacturing with the Formiga P 100 that afternoon and can send back the finished Platform the next day. This means about a 48-hour turnaround in the U.S., 72 to Europe.
Parts Consolidation
The EOS system has also enabled FHC to turn a number of creative thoughts into reality. “The freedom of design we can have with the Formiga allows us to make just about anything we can envision,” says FHC Founder and President Fred Haer.
 Fig. 5. Use of custom laser-sintered fixture (orange) for guided spinal surgery. |
Parts consolidation has been particularly successful. “We’ve been able to design-in additional features that simplify the mounting of various devices and reduce the possibility of assembly error,” he says.
One example is a metal indexing ring that was formerly screwed onto the Platform by the surgeon during the surgery. “Now we can incorporate that function within the finished fixture,” says Haer. “This saves FHC the effort of having to provide that machined part separately, and saves the hospital OR time because they don’t have to sterilize the part and keep track of small, loose screws during surgery.”
Future Potential
Other avenues FHC is exploring with the EOS system include building the tray of set-up tools for a case alongside the corresponding Platform, creating a fully disposable pre-sterile pack, and developing a living hinge for a part that holds the DBS electrode in place for testing. Going beyond the skull, the company is interested in expanding the development of enabling products in other surgical specialties such as orthopedics, where STarFix technology could be used to develop implant or fusion templates.
“We anticipate even greater product improvement opportunities from laser sintering as we go forward,” says Haer. “Having the flexibility of a technology that can create patient-specific solutions rather than one-size-fits-all can result in both hospital economies and better patient outcomes.”
Lynn Manning is a science and technology writer who wrote this article on behalf of EOS. Send comments about this article to [email protected].
More Info
For more information on this topic, visit deskeng.com.
Subscribe to our FREE magazine, FREE email newsletters or both!
Latest News
About the Author
DE’s editors contribute news and new product announcements to Digital Engineering.
Press releases may be sent to them via [email protected].


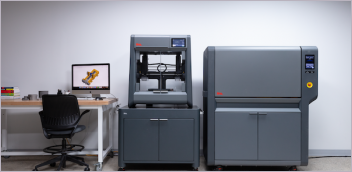



 Fig. 6. Representative neural recordings from an electrode track while targeting the subthalamic nucleus. Abbreviations: Th - thalamus; Re - reticular nucleus of the thalamus; Zi - zona incerta; STN - subthalamic nucleus; SN - substantia nigra. Reprinted with permission from Deep Brain Stimulation for Parkinson’s Disease: A Comprehensive Text (Baltuch, G.H., Stern, M.B., eds.), pp 93-102. New York: Informa Healthcare
Fig. 6. Representative neural recordings from an electrode track while targeting the subthalamic nucleus. Abbreviations: Th - thalamus; Re - reticular nucleus of the thalamus; Zi - zona incerta; STN - subthalamic nucleus; SN - substantia nigra. Reprinted with permission from Deep Brain Stimulation for Parkinson’s Disease: A Comprehensive Text (Baltuch, G.H., Stern, M.B., eds.), pp 93-102. New York: Informa Healthcare