Modern Stent Gets Medical Makeover
CFD modeling and visualization software help improve the safety and efficiency of this life-saving device.
Latest News
September 1, 2010
By Mike Peery
Coronary stent installations were once regarded as miracles of modern medicine. Today, they are viewed as reasonably low-risk, commonplace procedures—with more than 1 million patients receiving stent implants every year in the U.S. alone.
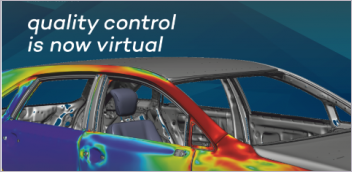
 This image shows the surface contour map of drug concentration in a bifurcating artery. A drug is released from the surfaces of the stent, where the red color indicates regions of more drug and blue indicates low drug concentration. The insets show high magnification images of the drug pattern (A) on the lateral wall of the main branch and (B) near the region where the flow divides at the bifurcation. This was created with Tecplot 360, a CFD visualization tool that helps to analyze and understand complex simulation data. Image courtesy of Tecplot |
In many cases, stents are lifesavers. But side effects such as post-procedure blood clots and heart attacks are still too common. Research in this area is rigorous and ongoing; however, it is often hampered by the complexities of the human arterial system, the wide array of variables presented in each individual case and the amount of data that must be weighed and analyzed.
This is where computational fluid dynamics (CFD) modeling and visualization methods are being put to good use: They help scientists efficiently manage and analyze data, and ultimately improve the safety of stents. In fact, some very exciting, pioneering work is being done at a number of major universities, including the Massachusetts Institute of Technology (MIT), with CFD modeling and visualization techniques playing a key role in that work.
Dr. Elazer R. Edelman, professor of health sciences and technology at MIT and professor of medicine at Harvard Medical School, is working alongside Dr. Vijaya B. Kolachalama, postdoctoral associate at the Edelman Laboratory at MIT, to revolutionize the world of heart therapy using CFD modeling, bench-top experiments, animal modeling and visualization.
 Visualizing a stent model. Image courtesy of Tecplot |
The two researchers are presently trying to get a better understanding of why stents, and the drugs delivered from those stents, can treat arteries on the one hand and cause blood clots on the other. They hope this research will eventually give doctors the ability to predict whether specific arteries with stent implants are at risk of blood clots.
Edelman and Kolachalama also hope their research can help medical device companies develop safer, more effective stents; aid in the regulatory approval process; and ultimately lead to the ability to design customized stents for each patient.
The Role of the Stent
To understand the importance of this work, it’s useful to understand the role that stents play in the treatment of heart patients and the problems they pose. Surgeons typically perform an angioplasty to reopen a blocked artery. They insert a catheter into the patient’s artery, and then inflate a balloon at the end of that catheter to compact atherosclerotic plaque against the artery walls. They then insert a stent—a small, metal-mesh tube—to keep the plaque from snapping back into the artery. As part of the healing response, tissue grows over the stent. In 25% to 50% of cases, however, this response is so severe that flow through the artery becomes sufficiently blocked, often requiring another procedure.
To prevent re-blocking, scientists began coating the stents with drugs, frequently embedded in a thin polymer material for time release. Called “drug-eluting” stents, these implants have reduced the need for repeat procedures to less than 10%. But even though the drug-eluting stents prevent tissue and plaque blockage, they create different issues for a small percentage of patients—resulting in life-threatening side effects like blood clots and heart attacks.
This problem lies with the way the metal-mesh stents must sit in the artery where they deliver their drugs. The stent lies against the wall of the artery, but still protrudes into the artery lumen. The mesh-like structure of the stent creates alternating flow disruptions, similar to the way rocks create whitewater in a flowing stream. The infused drug comes off the mesh struts at high concentrations and, once released, becomes subject to areas of high and low flow. As a result, the drug is distributed and deposited within the artery wall in a non-uniform fashion and, although it is governed by classic flow equations, its flow is non-intuitive and virtually impossible to predict. This issue becomes even more complex to understand when stents are placed at locations such as arterial branch points or tortuous vessels. It is now believed that these heterogeneous drug distribution patterns, with areas of extremely high drug concentration alternating with areas virtually depleted of drug, contribute to the localization of blood clots.
Addressing Flow Dynamics
While valuable data related to the biologic response to stents and drugs can be obtained through human trials and animal experiments, it’s difficult to examine the issues of drug distribution variability from these studies alone. Most current imaging technology is not sophisticated enough to offer a complete view of the drug patterns. In addition, individual patient variability renders it virtually impossible to track the large number of variables at play. Even subtle differences in the geometry of arteries or native disease, amount of drug delivered, change in drug absorption, or the way the stent is implanted can have dramatic effects in drug uptake.
Medical researchers are able to take what they learn from clinical experience and animal models—as well as bench-top studies—to create physiologically relevant fluid dynamic models. According to Edelman and Kolachalama, this is the ultimate use of CFD modeling and visualization.
Visualizing the Results
Edelman and Kolachalama are able to gather biometric data from several sources and in many formats to create mathematical models, which can then be solved against multiple variables or parameters. The simulation results, however, are in numerical format, making it nearly impossible for the human brain to interpret.
But by using sophisticated post-processor visualization software, researchers are now able to generate visuals that clearly show how the artery and drugs would behave under different conditions—similar to looking at the visual results from an X-ray or video scope. The resulting images provide insight into how drugs deposited from a stent are affected by numerous factors, including the positioning of the stent, changes in blood flow where arteries meet, and blood flow changes created by the stent itself.
These scientists expect CFD modeling and visualization tools, combined with other technologies like MCAD, will continue to help improve both the safety and effectiveness of stent implants. This can give researchers the means to study stent placement in arteries in a manner not possible before—and that has tremendous implications for engineers as they develop new devices designed to reduce life-threatening complications. Edelman and Kolachalama also hope to use these methods to streamline the regulatory process by giving regulatory bodies the information they need to determine whether proposed changes to stent technology are large enough to require a new clinical trial.
Ultimately, the researchers’ work with CFD modeling and visualization will assist physicians in making better “in-the-moment” decisions for patients. With different artery scenarios for each patient, scores of stent types and brands, and short timelines with which to make critical, life-saving assessments and judgments, doctors will be able to quickly sort through mountains of data to select the best stent and placement for a particular patient—based on fact, rather than perception.
These techniques will eventually allow doctors to use computers to compile all the options available, input them along with a patient’s medical data into a virtual artery and—like a GPS system that sorts a driver’s route—analyze and interpret the universe of variables and optimize the stent intervention. With help of CFD modeling and visualization, the process will become supremely accurate and efficient, resulting in an even better outcome for the patient.
More Info:
Massachusetts Instituteof Technology
Tecplot
Mike Peery is the co-founder and CEO of Tecplot, Inc. He has more than 30 years of technical and managerial experience in the development of software products for CFD analysis and scientific/engineering data visualization. Contact him via [email protected].
Subscribe to our FREE magazine, FREE email newsletters or both!
Latest News
About the Author
DE’s editors contribute news and new product announcements to Digital Engineering.
Press releases may be sent to them via [email protected].